Most Healthcare Workers Are Excited To Get A Coronavirus Vaccine, But Some Have Questions
Healthcare workers are at the front of the line to receive the United States’ first coronavirus vaccine. But hospitals have a challenge: Not all of them are thrilled to be there.
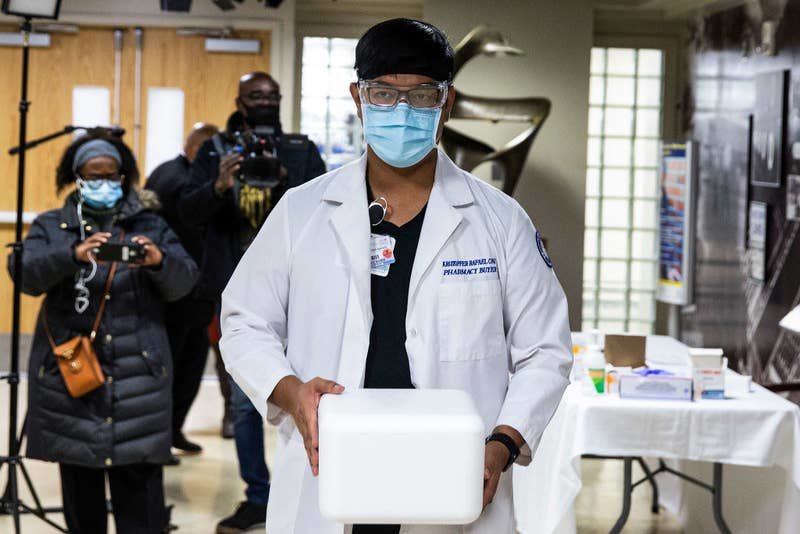
Amid a raging pandemic that has now killed more than 300,000 Americans, the vaccine, made by Pfizer and the German company BioNTech, is a beacon of hope. Authorized for emergency use by the Food and Drug Administration on Friday, millions of doses will arrive in all 50 states this week, kicking off the most ambitious immunization campaign in US history. To start off, the CDC recommends giving first priority to the most vulnerable groups: people at long-term care facilities and the nation’s 21 million healthcare workers.
After an exhausting year in which caseloads crushed emergency rooms across the country, many, if not most, doctors and nurses are ecstatic that a highly effective vaccine has arrived. Another equally promising vaccine, by the company Moderna, is expected to be greenlit this week, bringing even more relief.
On Monday, a New York City critical care nurse named Sandra Lindsay became the first American to get Pfizer’s vaccine outside of a clinical trial. Her message was clear: “I want to instill public confidence that the vaccine is safe.”
“Definitely I will be getting a vaccine, and I will be getting it publicly,” Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, said late last week. “I think that the data looks great. I’m excited about it. I think it’s a huge win for science,” Krutika Kuppalli, an infectious diseases physician at the Medical University of South Carolina, told BuzzFeed News, before getting vaccinated on Tuesday. Hospital staffers have been filling social media with joyous posts in anticipation of their shots.
But those who work in healthcare settings are not exempt from feeling skeptical or fearful about getting the new vaccine, according to surveys.
Healthcare workers appear to be moderately, but not overwhelmingly, willing to get vaccinated, a CDC advisory panel acknowledged last weekend. In a separate CDC survey this fall, 63% of providers said they’d get vaccinated. In an October survey of nearly 13,000 nurses, conducted by the American Nurses Foundation, about two-thirds of respondents said they were unsure or would not voluntarily get a vaccine. And several hospital networks acknowledged in interviews with BuzzFeed News that, while the majority of their staffers are enthusiastic about getting vaccinated, some have reservations.
Ralph Wang, an emergency medicine physician at University of California, San Francisco, is hopeful that he and his family can be protected from COVID-19 — but, he said, this shot feels different from something as familiar as the flu vaccine. “I’ve gotten it before. Millions of people have gotten it before,” Wang said. It’s the “newness” of the coronavirus vaccine, he explained, that “gives me pause.”
Ultimately, Wang said, his concerns are unlikely to outweigh the positives of helping protect his workplace, his family, and his community against a deadly virus.
“If someone told me, ‘Ralph, you have to decide right now,’ I would probably say yes,” he concluded.
Public health experts say that acknowledging and responding to these concerns in a transparent way will be important for building public trust in coronavirus vaccines as they are rolled out nationwide. And they say that the gap in trust reflects a failure of the federal government — which poured $14 billion into an effort to rapidly develop and manufacture COVID-19 vaccines — to also invest in public awareness about how the shots work, how they were vetted, and what’s known about safety.
That public-private partnership, Operation Warp Speed, “has been a great program in terms of scientific rigor and integrity of the clinical trials, but it was never linked to a major program of communications,” Peter Hotez, a vaccine expert at Baylor College of Medicine, told BuzzFeed News in an email. The resulting information vacuum was often filled by corporate press releases aimed at shareholders and by the online anti-vaccine movement, he said.
None of the hospitals interviewed for this story said they would require their employees to get the vaccine, citing a belief that a mandate would be both impractical and likely to backfire. Instead, they are hoping to get staffers on board voluntarily by answering questions, distributing information in various formats, making shots widely available, and encouraging those who get inoculated early to share their experiences with their peers.
“It’s going to be a marathon,” said Susan Mashni, head of the vaccine distribution task force at Mount Sinai Health System in New York City. Mashni said 60% of doctors throughout the hospital network, and half of nonphysicians, noted in a recent survey that they’re enthusiastic about the vaccine. “If folks don’t feel comfortable right now, hopefully they’ll come back and feel comfortable with some time.”
Convincing doctors, nurses, and others of the importance of immunization will be crucial for the bigger task of swaying the public, which is expected to start getting vaccinated in April. To stop the virus’s spread, experts say, 60% to 70% of the population will need to recover from COVID-19 or get vaccinated. In a recent Pew Research Center poll, about 40% of respondents said they “definitely” or “probably” would not get a vaccine, though about half of that group added that it’s possible they would get vaccinated once others do so and more information becomes available.
That makes the early rollout of the vaccine to healthcare workers even more crucial: Family physicians, studies have shown, can be a powerful influence on parents who are hesitant about vaccinating their children. The same could be true for making sure the majority of Americans get the COVID-19 vaccine.
“We encourage physicians to learn all they can,” said Susan Bailey, president of the American Medical Association, “because if we don’t have complete confidence in the vaccines, we’ll never convince our patients to have complete confidence.”
Pfizer’s vaccine is the fastest vaccine in history to make it from the lab to the public. It is also the first authorized vaccine to be made from the genetic molecule messenger RNA (mRNA), which instructs human cells to make proteins that prime the immune system to recognize and attack a coronavirus infection. In a large late-stage clinical trial, the vaccine was 95% effective at preventing infections, a rate that exceeded many scientists’ expectations. The vaccine was also found to be very safe, with no serious side effects.
Those qualities make the vaccine “one of the greatest scientific accomplishments in history,” as President Donald Trump put it after the FDA issued its authorization on Friday. Moderna’s vaccine also uses an mRNA-based platform and is 94% effective at preventing symptomatic illness, according to data released and confirmed by the FDA on Tuesday.
But to some people, the rapid development of those vaccines is troubling.
At the Medical University of South Carolina, where Kuppalli is helping coordinate the vaccine rollout, an employee asked her after a recent town hall: “If these things are so great, why were we able to do this in seven months?”
In response, Kuppalli pointed to the three decades of research on mRNA as a potential medical tool, including human clinical trials on other vaccine candidates based on that technology, in part backed by years of investment from the federal government. “This is a very intricate, difficult process they’ve finally been able to figure out,” she explained.
Because of the out-of-control outbreaks in the US, clinical trials for coronavirus vaccines were also able to quickly collect data that showed they worked. In Pfizer’s trial, 162 participants who received the placebo got infected; in the same time frame, only eight people who got the vaccine became sick.
The FDA said it had “no specific safety concerns” about Pfizer’s vaccine, based on more than 18,000 trial participants who had received it. But mild side effects were common: About a quarter of participants experienced some kind of reaction, most commonly arm soreness, fatigue, headaches, muscle pains, chills, joint pain, and fever. No serious side effects were linked to the vaccine. While two months of safety data have been reported so far, Pfizer will continue tracking participants for signs of side effects for two more years.
But Wang, the UCSF physician, is worried about the possibility of side effects so rare they’ll only show up once millions start to be vaccinated. Such incredibly rare side effects are to be expected for any new drug or vaccine: For instance, for every 1 million flu shots, the risk of Guillain-Barré syndrome, an immune disorder that can result in paralysis, is thought to increase by one or two cases. “That’s a 1 in a million consideration, which we won’t know about [with the coronavirus vaccine],” Wang said.
A nurse practitioner at New York University’s Langone Medical Center, who requested anonymity because they were not allowed to speak to the press, also expressed concern about the unknowns, a reluctance they felt toward “any new medication.”
“The reality is we don’t know a lot of long-term side effects,” they said. “There may not be any, but we’re not going to know that for a while.”
There are open questions about ultrarare or long-term side effects — and then there’s the vast amount of COVID-19 misinformation spreading online. Since day one of the pandemic, social media platforms have been battling accounts that share out-of-context information, misconceptions, and flat-out falsehoods about the virus and, now, the vaccines.
One recent rumor, for instance, claimed that Pfizer’s head of research said its vaccine would make women infertile. It was started by a blog called Health and Money News, flagged in Facebook’s efforts to combat misinformation on its platform, and decisively debunked by PolitiFact, the Associated Press, and the New York Times.
“I don’t even know how this stuff gets made up,” said Serena Bumpus, director of practice at the Texas Nurses Association. “It’s those sorts of things that we need to help people filter out and really pay attention to what we know to be true.”
Even before the pandemic, vaccine hesitancy was identified by the World Health Organization as one of the top threats to global health. And some of the public messaging around the coronavirus vaccines hasn’t helped restore confidence.
“Operation Warp Speed” was a name that seemed to prioritize speed over safety. Trump pressured the FDA to approve a vaccine before the November election and contradicted timelines given by his own health officials. And Kamala Harris, as a vice presidential candidate, said she would not take a vaccine endorsed by Trump alone.
The pharmaceutical companies haven’t always helped their own cause. Pfizer and Moderna made public their typically secret clinical trial blueprints, but only after scientists urgently called for greater transparency. And both companies released their promising data in press releases, not peer-reviewed studies. (Last week, the FDA did release its independent analysis of Pfizer’s data, and the company published its results in the New England Journal of Medicine.)
More recently, when AstraZeneca and Oxford University published a press release announcing results from late-stage clinical trials of their vaccine, they presented a range of efficacy rates for different dosing regimens. But some outside scientists say that they were not transparent about how the trials were conducted and that they had spun their data to present more impressive results.
A lot of healthcare workers have the added hurdle of personally experiencing unequal health treatment, said Sheria Robinson-Lane, a professor at the University of Michigan School of Nursing. About 1 in 5 registered nurses, and 29% of vocational nurses, identify as a racial or ethnic minority.
“We often don’t think of them as low-wage workers, but in many instances they are. Many of them have poor access to health insurance, so many of them have seen the most devastating effects of COVID,” Robinson-Lane said. In the case of a vaccine, “when people say, ‘Let’s test it, and it needs to go to Black folks first,’ people don’t necessarily look at that as a positive sort of thing. They go back to this idea of not wanting to be guinea pigs, so to speak.”

Someday, hospitals could conceivably require employees to get immunized against the coronavirus. There is legal precedent, experts said: Some hospitals already mandate some immunizations, like the mumps, measles, and rubella vaccine and a yearly flu shot.
But for now, Pfizer’s vaccine is still experimental. It will be available under an “emergency use authorization” from the FDA, which is based on less data than a full approval. “Folks have to have the freedom to consent to a drug that’s not FDA-approved,” said Mashni of the Mount Sinai Health System.
Employees would almost certainly resist any vaccine mandate at this stage, hospital directors said. “It’s not even a discussion right now,” said Christine Turley of Atrium Health, a 70,000-employee hospital network in North and South Carolina and Georgia.
“I can’t envision anybody doing that here,” said Deb-Fischer Clemens, president of the South Dakota Nurses Association. “In South Dakota, we tend to not trust government, and there’s quite a population here that is not wanting anyone to tell them what to do.”
That said, she thought that most nurses in her state, where waves of critically ill patients are overwhelming intensive care units, are excited to get a vaccine. As for the rest, she said, “We just have to educate.”
Saad Omer, an expert in strategies to combat vaccine hesitancy and director of the Yale Institute for Global Health, said the most effective public health messaging will need to come from the top.
In an analysis of surveys conducted in September, Omer and his colleagues found that a bipartisan endorsement of a vaccine from Democratic House Speaker Nancy Pelosi and Trump would encourage people to take it. Fauci’s endorsement would be even more persuasive to respondents of all political affiliations, the study found.
Omer also said that the federal government should run a national education campaign that delivers basic facts about vaccination to the public. “That hasn’t happened,” he said. “That could help at a big-picture level.” The Trump administration is now launching such a campaign — initially delayed because of concerns that the president was using it to boost his chances of reelection — and President-elect Joe Biden is working on his own messaging plan.
In the meantime, hospitals have been mounting their own education efforts. Mount Sinai is posting information for its employees internally, distributing FAQ sheets, compiling videos and PowerPoints, hosting town halls, and printing palm-sized cards with talking points to be carried around in case conversations arise, Mashni said.
Christus Health, a Catholic health system based in Texas, is working with an internal group of physicians dedicated to addressing health inequities to get the word out to communities of color about the vaccine, said Sam Bagchi, the nonprofit’s chief medical officer. In an employee survey, he said, one-third of respondents said they wanted the vaccine, 40% were unsure, and the rest said they weren’t interested.
Some of Christus’s staff members were in the clinical trials, and Bagchi is working on having them share their experiences with the rest of the organization “so that it’s not me as a leader, it’s not the federal or state government, but it’s somebody’s peer, somebody that looks like them, somebody that’s from their same care area or from their same geography,” he said. “They got the vaccine, it wasn’t that bad, and their arm hurt for a while — but now they’re feeling better, and they’re excited that they did it.”
In these conversations, people should be open about the fact that no vaccine is a panacea, experts said. “There tends to be a lack of information that’s made available regarding both the good and bad things with vaccinations,” Robinson-Lane said. “We talk about all of the benefits, but we don’t necessarily talk about some of the side effects or concerns.”
And Omer pointed out, “There is no absolute safety in anything. It is a risk-versus-benefit ratio, and that’s a fact of life, unfortunately. And the key is in the middle of a raging pandemic that sees mass mortality on a daily basis. What is the risk-versus-benefit ratio of these vaccines?”
Managers should not just warn employees about the possibility of side effects that surface in the days after their shots, but plan for it. Staffers should stagger getting the vaccinations for themselves so people can take time off without jeopardizing medical care for patients, some experts say.
Above all, people need to be compassionate and patient in persuading others, said Craig Spencer, an emergency physician at New York-Presbyterian/Columbia University Medical Center. “We all just assume that healthcare providers are a monolith and put science above all and think vaccines are the best things on the face of the earth,” he said. “But there’s obviously variability, even amongst frontline workers, in their personal experience, and we can’t undermine that.”
As Pfizer has released more data about its vaccine, Spencer said, he has come to find it “incredibly encouraging” and feels “really optimistic.” Having treated patients during New York’s grueling surge in the spring, and now once again this winter, he added, being vaccinated would “help with some of that mental exhaustion and that mental stress.”
Lately, Spencer has tried to spread some of that optimism to colleagues — nurses, technicians, security guards — who are approaching him with questions about the vaccine. He is confident that more people will get on board as they hear firsthand from friends who get vaccinated. “The people I work with in my emergency room, I’ve worked with them for nearly a decade. They trust me,” he said.
For others, the decision will be based not on personal interactions but an assessment of the facts. “As a doctor and someone who does research,” said Wang, “I always want to look at primary publications to look at how the studies were done and to have a look at the data for myself.”
And for all his concerns about the risks, the many potential benefits are not lost on him.
“As healthcare workers in emergency departments, we’ll be protected, and so our patients will be protected, and our families will be protected,” he said. “That’s why I would take the vaccine.”