What Hong Kong can learn from Singapore, UK, on welcoming overseas doctors
Following the initial reading of the Medical Registration Amendment Bill in the Legislative Council, public discussion of Hong Kong’s doctor shortage
crisis has returned in full force. The bill’s arrival is not without cause.
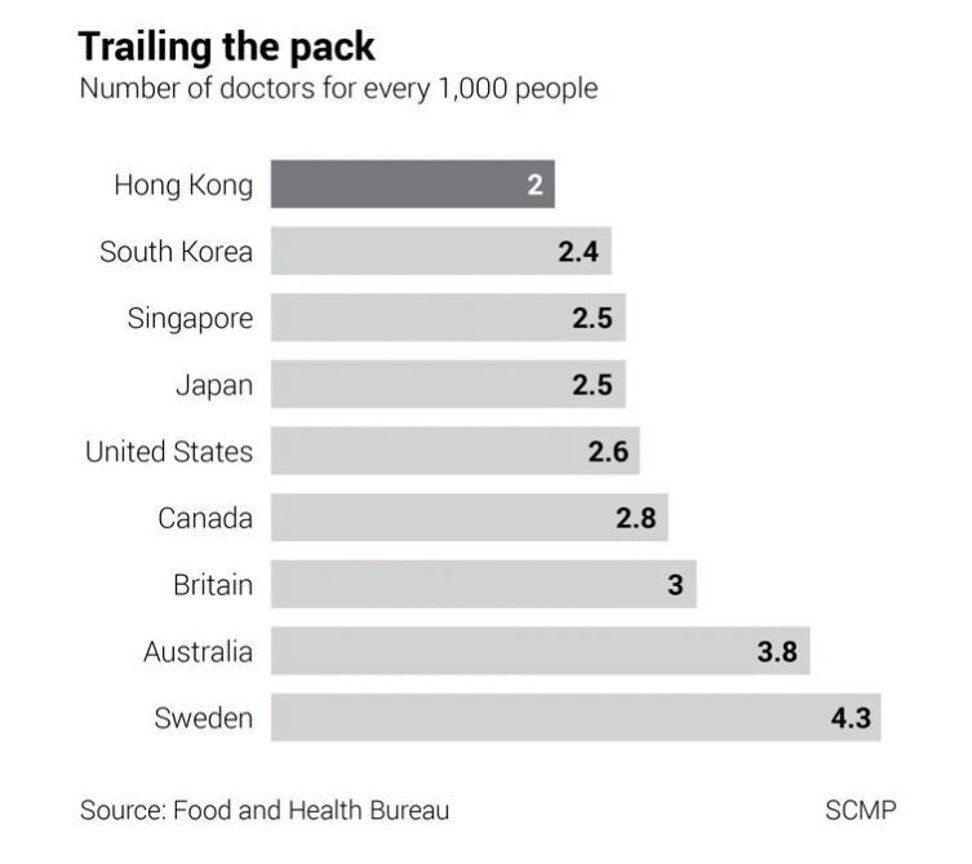
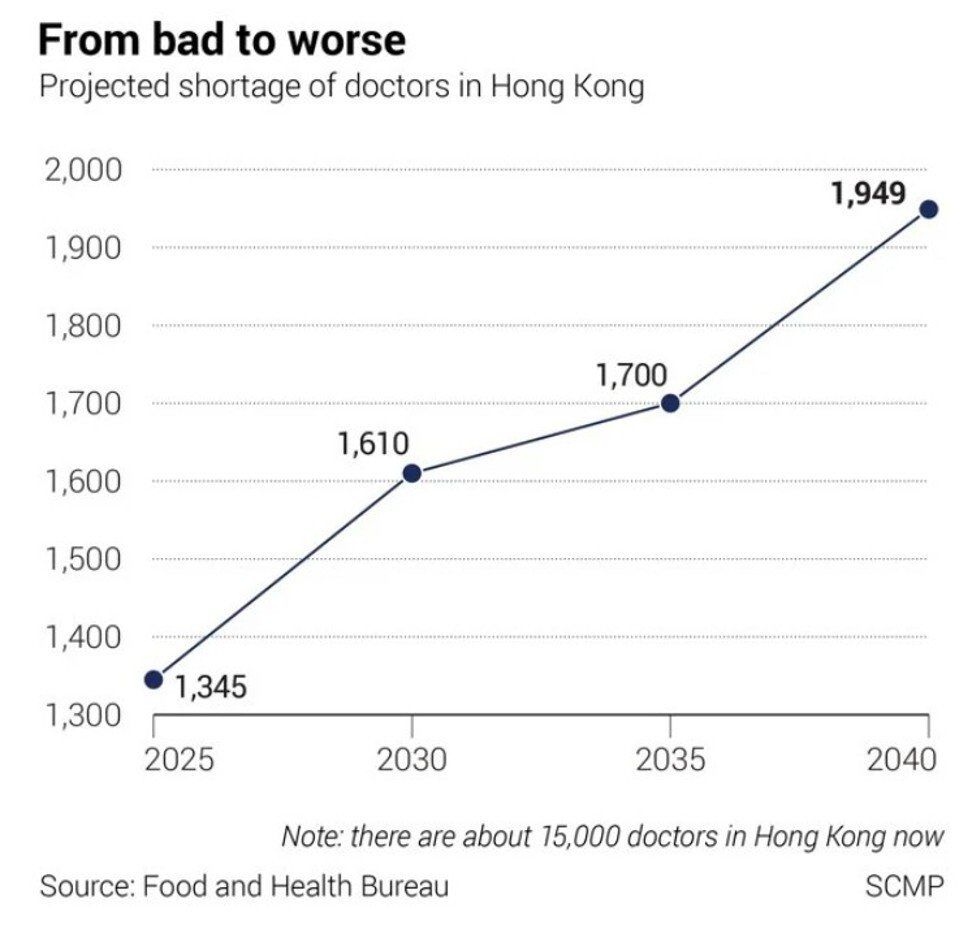
Latest government projections show Hong Kong faces a shortfall of 1,610 doctors by 2030, even after accounting for the yearly intake of newly graduated locals. Nonetheless, Hong Kong is not alone in its crisis.
Singapore and Britain have also faced doctor shortages but both have made significant strides in closing their gaps. Being flexible for entry into their health care systems has earned them higher doctor-to-population ratios than Hong Kong.
Notably, both systems welcome doctors,regardless of how far they have got in their specialist training. In both countries, non-locally-trained doctors have the option of full or partial specialist training.
Hong Kong’s newly formulated special registration pathway is being proposed for medical practitioners who have yet to start, are looking to continue, or have completed their specialist training.
With the new pathway in mind, how do Hong Kong’s current specialist training opportunities and recognition mechanisms compare with those of Singapore and Britain, and what can we learn from them?
A recently released report by Our Hong Kong Foundation, in which non-locally-trained doctors with limited registration were interviewed, identified difficulties these doctors faced in continuing specialist training and in the recognition of specialist qualifications.
Despite candidates having the necessary qualifications for employment and vacancies in training programmes, they reported that contractual limitations prevented them from accessing continuing specialist training. Various Hong Kong Academy of Medicine colleges, which oversee specialist training, have explicitly denied access to these doctors.
Experienced specialists in Hong Kong fare no better. Those seeking official recognition through the lesser-known Certification for Specialist Registration pathway, which has approved just 49 applications in the past decade, may still not be guaranteed equal career progression opportunities compared to locally trained specialists.
Furthermore, specialists under the limited registration scheme working in the Hospital Authority are only eligible for promotion to the middle rank of associate consultant in a limited number of specialities and are blocked from reaching the highest consultant rank.
The cumulative effect of these training barriers and unfair specialist recognition is that the environment has become patently unwelcoming to doctors hoping to enter and work in Hong Kong’s health system. Luckily, it does not have to be this way as it is not yet set in stone.
We only need to look to Britain or, closer to home, Singapore for guidance on how to offer clear-cut pathways to recognise prior training and equal career progression opportunities for non-locally-trained doctors.
 National Health Service staff pay tribute to their colleagues during the
national applause for the NHS outside Chelsea and Westminster Hospital
in London, on May 21, 2020. Like Hong Kong, the UK faced a doctor
shortage but has done a better job of recruiting medical professionals
from overseas.
National Health Service staff pay tribute to their colleagues during the
national applause for the NHS outside Chelsea and Westminster Hospital
in London, on May 21, 2020. Like Hong Kong, the UK faced a doctor
shortage but has done a better job of recruiting medical professionals
from overseas.
As recommended in the foundation’s report, to tackle the issue of specialist training, the Hong Kong Academy of Medicine (HKAM) should be further empowered to mandate higher quotas at each of its colleges, to allow more trainees in each programme.
The academy could further facilitate continued training through integrated contracts, which can provide flexibility for employment and training. The government should offer the academy and the Hospital Authority additional funding to ensure training can be provided to non-locally-trained doctors without affecting opportunities for locally-trained specialists.
To address the issue of specialist recognition, the government, Hospital Authority, and HKAM could combine efforts to ensure non-locally-trained specialists are treated fairly. For equitable career progression, the Hospital Authority should pledge to remove any barriers and allow promotion in all ranks and specialities, and determine progression based on merit.
The government can reference Singapore’s Specialists Accreditation Board and set up a similar independent body, with international experts, that is responsible for specialist accreditation and recognition.
Singapore’s board determines the qualifications needed for registration and the training programmes to be recognised. The board does well in explaining the requirements for specialists depending on where they did their training, leaving little room for confusion about the required qualifications.
Specialists also receive equal recognition to their locally-trained counterparts after assessment by the board, thereby giving them equal career progression opportunities. Similarly in Hong Kong, specialists should receive the same entitlements as their locally-trained peers.
Hong Kong, like many places, is facing a serious shortage of doctors, which will only grow worse if nothing is done to tackle the issue. The effects will be felt by people who experience long waiting times for health services.
When we look at the successes of Singapore and Britain in this regard, it’s clear that Hong Kong still has much to do to fix its health care and doctor issues. These other two systems are far from perfect, but their efforts showcase possible solutions to the crisis in our public health system.
We can better serve Hongkongers’ health demands only if we have the doctors to be able to do so. In looking to other places, we can map a way forward and aspire to do better.